We understand that you are concerned and worried about your loved one.
While we will try to accommodate you as much as possible, please remember that providing the patients on this ward with the best possible care is our primary objective.
To help us do this, we ask you to observe the following during your visit:
- We try to keep visiting times as flexible as possible (by prior arrangement) so that people with work commitments still have the opportunity to visit their relatives in the Unit. Patients on this ward are often seriously ill, and many of them have extremely challenging intensive care and treatment needs. As a result, we ask for your understanding at all times – you may need to wait before you can enter the patient’s room. And you may be asked to leave the room during your visit for medical reasons. Generally speaking, afternoons are more favourable for visits.
- The doctors on duty and specialist nursing staff should be available to answer any questions you may have about patients. For legal reasons, information can only be given to immediate family members without the patient's consent. Please note that only close relatives who are already personally known to us and who quote the patient-related password will be given information over the telephone. We ask that you try to limit telephone enquiries to between 9:00 and 10:00 in the morning and 19:00 and 20:00 in the evening.
As many of our patients are at risk of infection, visitors must observe certain hygiene measures:
The following applies to all visitors:
1. Thorough hand cleaning (washing hands with soap; drying them thoroughly) upon entering the ward. Subsequent hand disinfection and the wearing of a disposable PPE apron is also necessary to avoid spreading germs.
2. There should never be more than two visitors with a patient at the same time.
3. Unfortunately, potted plants and flowers are not allowed on the ward for hygiene reasons.
Visits by children under the age of majority (i.e. 17 or under) are subject to consultation with our team. There are only very limited storage options for patients' personal possessions in an intensive care unit. We kindly ask you to take any toiletries and items of clothing that are not absolutely necessary home with you.
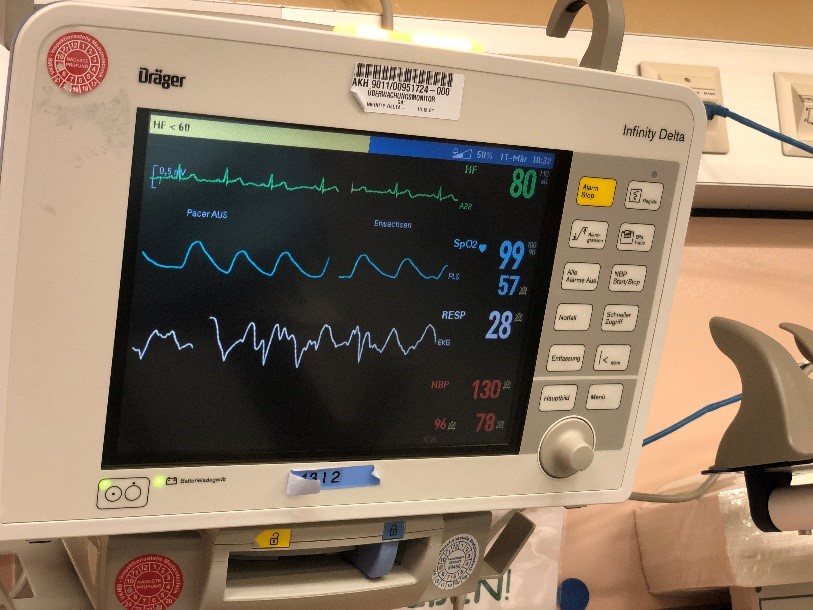
The many devices and cables around your relative are certainly unfamiliar and may be quite alarming for you at first glance. We would therefore like to give you a brief overview of what they all do.
In principle, they are there to monitor and support of the patient’s most important bodily functions: adhesive electrodes attached to the upper body determine the heart rate (green line on the monitor) in real time. The results are displayed on a monitoring device, both at the bedside and in the ward control centre. This device runs around the clock and provides a notification if the heart rate becomes too fast or too slow. Please note that false alarms are also possible, e.g. if the patient moves in such a way that the adhesive contacts pick up an incorrect reading. Another sensor is used to measure the SpO2 value (blue line on the monitor screen), which is a parameter that is used to monitor the patient's oxygen supply.
The respiratory rate is also recorded (white line on the monitor). Thin plastic tubes (catheters) placed in arteries and veins may also be used for constant monitoring of blood pressure, temperature and other vitals. Medication and nutritional fluids may also be fed directly into the bloodstream via catheters, and blood is taken from them for examination purposes.

Where gastric decompression is necessary, many patients have a thin nasogastric tube inserted through a nostril into their stomach. This type of tube is also used to provide liquid nutrition to the gut.
In order to support – or in some cases replace – lung function, some patients have to be artificially ventilated. A ventilator takes over their breathing entirely or helps the patient inhale and exhale through a tube that leads through the mouth into the windpipe. As the tube runs through the glottis (voice box), your relative will be unable to speak in this situation. Ventilation is often perceived as unpleasant, so sedatives and painkilling medication may also be administered. Sometimes the patient will require general anaesthetic and be placed in an induced coma.

In some cases, a tracheotomy may be needed when a ventilator is required for breathing. This is a routine procedure that lasts around half an hour. It is mainly used in situations where patients depend on a ventilator for an extended period. In such cases, the normal breathing tube can be removed from the mouth and throat. Patients can then be ventilated via a smaller tube through the throat.
Positioning therapy is carried out to ensure an even distribution of oxygen within the artificially-ventilated lungs. Lateral (i.e. laying on the side) and prone (on the stomach) positions are a normal and important part of the treatment procedure and not a cause for concern.
If your relative is awake, they need a great deal of care and support from us – and especially from you. We need to explain the situation to them and take a lot of time to ensure that they are able to make themselves understood.
In this context, we think that due consideration should be given to the commonly-asked question of whether it makes sense to visit a relative when they are unconscious. Although it is not possible to prove it, our belief is that your relative does in fact register your voice and touch and benefits from it, even if they are not actually able to confirm that themselves.
Especially during unconsciousness and the wake-up phase, we ask relatives to keep a very close eye on the number of visitors that the patient receives. We understand that many family members as well as people in their circle of friends will feel the need to visit the patients in our care. But we ask you to coordinate visit carefully with one another. In our experience, it is very stressful for both patients and for you if visitors end up having to take turns at the patient's bedside and switching every five minutes. A more sensible approach would be a daily roster of visitors, overseen by the next of kin. Thank you in advance for your co-operation in this regard!
We would like to point out that filming and photography in hospital rooms is only permitted with the prior approval of the hospital administration in accordance with hospital management’s guidelines. Please note that employees of the hospital may not be photographed or filmed without first obtaining their express consent.
Mobile phones can cause interference with medical devices. For safety reasons, use of mobile phones, smartphones, tablets and similar devices by relatives is strictly prohibited in the intensive care unit. Please switch electronic devices to flight mode or turn them off completely before your visit.
We ask for your understanding that we cannot accept any liability for any items left in the cloakroom or other valuables that you bring onto the Unit with you.
Your relative's stay in the Unit is a very difficult and unsettling time for you. We understand your concerns and hope that this introduction has been of some assistance. Our team will be happy to answer any further questions or concerns you may have.
Your 13i2 Team
